Urinary incontinence in women is a common problem that can have a significant impact on the quality of life.
This condition refers to the inability to control urine and can appear in different ways. In the following, we explain its types, causes and treatment methods:
Types of urinary incontinence
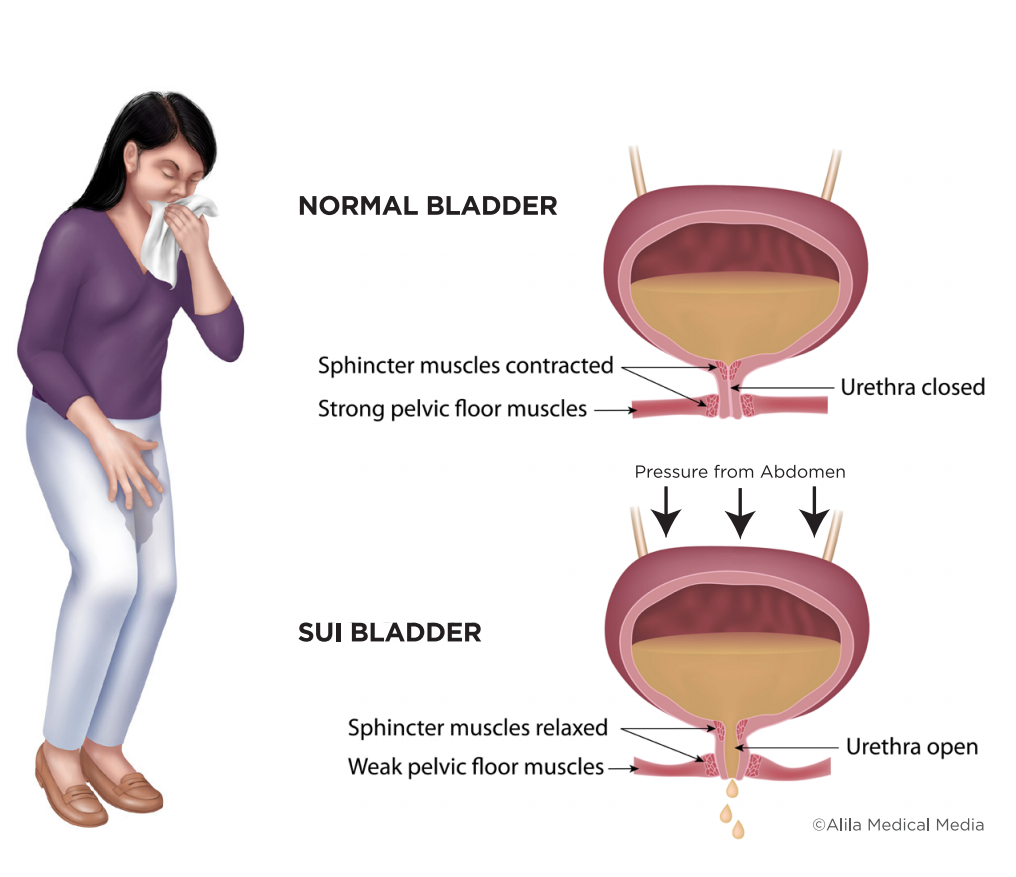
1.Stress incontinence:
Caused by pressure on the bladder during activities such as coughing, sneezing, laughing or exercising.
It usually occurs due to pelvic floor muscle weakness or hormonal changes after childbirth or menopause.
2.Urgent incontinence:
A sudden and strong urge to urinate, leading to leakage of urine.
It may be due to infection, inflammation or nerve problems.
3.Mixed incontinence:
A combination of stress and urgency incontinence.
4.Overflow incontinence:
When the bladder does not empty completely, causing urine leakage.
It is usually due to nerve problems or urethral obstruction.
Causes of urinary incontinence
Childbirth: Natural childbirth can damage the pelvic floor muscles.
Menopause: The decrease in estrogen hormone can affect the tissues of the bladder and urethra.
Genetic factors: family history may play a role in the occurrence of this problem.
Obesity: Excess weight puts more pressure on the bladder.
Chronic diseases: Diabetes, neurological diseases or bladder infections can lead to incontinence.
Treatment methods
Kegel exercises:
Strengthening the pelvic floor muscles that can help control urination.
Medicines:
Some medications can help reduce the symptoms of incontinence.
Changes in lifestyle:
Reducing the consumption of caffeine and liquids before sleep, weight loss and stress control.
Medical treatments:
In severe cases, surgery or microbiological treatments may be required.
Counseling and psychotherapy:
In some cases, counseling can help manage the psychological side effects of this problem.
conclusion
Urinary incontinence is a treatable problem, and seeing a doctor can help find the best treatment options.
Awareness and acceptance of this situation can be the first step to improve the quality of life.
Additional tips about urinary incontinence
1. The role of counseling and psychological support
Urinary incontinence can have significant emotional and psychological effects. Many women may feel ashamed or anxious, and this may affect their social relationships and quality of life.
Counseling and support groups can help people deal with their feelings and find ways to manage their condition.
2. Tests and diagnosis
To accurately diagnose the type of incontinence, the doctor may perform the following tests:
Medical history: questions about symptoms, medical history, and living conditions.
Urine tests: to check for infections or bladder problems.
Physical check-up: examining the condition of the pelvic floor muscles and sensitive points.
Urine flow study: to evaluate the manner and amount of urine discharge.
3. Prevention
Although some factors such as age and genetics cannot be changed, urinary incontinence can be prevented by following some tips:
Strengthening pelvic floor muscles: Kegel exercises help to strengthen these muscles.
Weight control: Maintaining a healthy weight can reduce pressure on the bladder.
Avoiding smoking: Smoking can lead to respiratory problems and chronic cough, which itself causes incontinence.
Healthy diet: Consuming enough fruits, vegetables and fluids helps maintain bladder health.
4. Auxiliary products and tools
If urinary incontinence is severe, the use of assistive products such as absorbent pads or adult diapers can help with daily comfort.
These products are designed to provide comfort and confidence to people.
conclusion
Urinary incontinence in women is a common and treatable problem that needs attention and treatment.
With medical support and lifestyle changes, many women can improve their symptoms and improve their quality of life.
It is important to take this matter seriously and see a doctor if necessary to find the best solutions for management and treatment.

5. Examining new and innovative treatments
In recent years, a number of new and innovative treatments for urinary incontinence have been developed that can help patients:
Nerve stimulation: Treatments such as sciatic nerve stimulation or transcutaneous nerve stimulation can help reduce incontinence symptoms.
These procedures are usually non-invasive and can help improve bladder function.
New drug treatments: Some newly introduced drugs can help relieve symptoms of urge incontinence. These drugs usually have fewer side effects and can be used for long-term management.
Advanced surgeries: In severe cases, surgeries such as sling surgery or bladder reconstruction surgeries can effectively treat urinary incontinence.
6. Education and awareness
Education about urinary incontinence and its causes is very important. Many women do not know enough about this and may feel ashamed to talk about it.
Holding workshops and training sessions can help increase awareness.
7. The effect of lifestyle on urinary incontinence
Lifestyle plays an important role in managing urinary incontinence. The following can help improve the situation:
Regular exercise: Regular exercise can help strengthen pelvic floor muscles and improve urinary control. Low-stress exercises such as walking, yoga, and swimming are also helpful.
Stress management: Stress can worsen incontinence symptoms. Stress management techniques such as meditation, breathing exercises, and relaxation exercises can help reduce symptoms.
Adequate sleep: Proper and adequate sleep can help improve general health and especially bladder health.
8. Final conclusion
Urinary incontinence is a common problem that can have profound psychological and social effects. But with knowledge, awareness and proper treatments,
many women can have more control over their condition. Encouraging talking about it and getting medical help can help improve quality of life and reduce anxiety.
Finally, if you or someone you know is experiencing this problem, it is important to see a doctor to find appropriate and effective ways to manage the condition.
9. Research advances and future treatments
Research on urinary incontinence is progressing rapidly. Some new research areas include:
Gene therapy: Research is investigating whether gene therapy can help improve bladder function and urinary control. This approach can be a solution for treatment-resistant incontinence.
Developing vaccines: Some researchers are working on vaccines that may help boost the immune system against infections that cause incontinence.
Nanotechnology and new materials: The use of nanotechnology in the production of new sanitary products can help design absorbent pads
and diapers that are more comfortable and effective.
10. The role of doctors and health professionals
Doctors, nurses and other health professionals play an important role in the diagnosis and management of urinary incontinence. They can:
Education and counseling: Educate and guide patients about treatment options and management of this problem.
Accurate diagnosis: identify the type of incontinence and its underlying causes by using appropriate tools and tests.
Emotional support: Help patients deal with negative feelings related to incontinence and encourage them to talk about their condition.
11. Practical tips for daily management
Women with urinary incontinence can help improve their condition by observing the following tips:
Planning to use the bathroom: Establishing a routine for going to the bathroom regularly can help reduce symptoms.
Using sanitary products: Using special pads or diapers can help with comfort and confidence.
Self-care: Attention to general health, including proper nutrition and regular exercise, can help improve bladder health.
12. Summary and final conclusion
Urinary incontinence is a complex problem that can occur for various reasons and have profound effects on individual and social life.
However, this problem is treatable and there are several options to manage and improve it.
Awareness, education and conversation about urinary incontinence can help break taboos and increase social acceptance.
Finally, if you or someone you know is experiencing this problem, it is important to see a doctor and get professional advice.
Despite the challenges, many women can improve their quality of life by receiving appropriate treatment and continue to live active and fulfilling lives.
13. Social support and resources
Social support can play an important role in managing urinary incontinence. Support groups and social networks can help people feel less alone and share their experiences with others:
Support groups: Joining local or online groups can help people connect with others who are having a similar experience and share helpful tips and tricks.
Websites and Online Resources: Many organizations and foundations provide detailed information about urinary incontinence.
These resources can include counseling, therapeutic information, and scientific articles.
14. Use of technology
Technology can help manage urinary incontinence. Some tools and apps can help people track symptoms and manage the condition:
Health apps: These apps can help users record their toilet times, fluid intake, and symptoms. This information can help doctors in better diagnosis and treatment.
Smart devices: Some wearable devices can help monitor symptoms and send data to the doctor.
15. The future of urinary incontinence
Medical and research advances are changing the way urinary incontinence is managed. In the future, we may see more innovative solutions that can solve this problem more effectively:
Early detection: Advances in diagnostic technology can help detect bladder problems and incontinence early.
Personalized treatments: Due to advances in genetics and pharmacology, treatments may be tailored specifically for each individual.
16. The final message
Urinary incontinence is a common problem that should not be treated as a taboo or non-negotiable issue.
With increased awareness, education and access to appropriate resources, women can manage this problem and improve their quality of life.
If you or someone you know is struggling with urinary incontinence, it’s important to seek help from your doctor and take advantage of available treatment options.
Also, supporting each other and talking about this issue can help break the silence and reduce the stress caused by this problem.
Finally, we must remember that urinary incontinence is a part of life for some people, and with the right treatment and support, you can continue to live a healthy and fulfilling life.
17. Urinary incontinence concerns
Although urinary incontinence is a common problem, some women may be embarrassed to talk about it or worry about its social and psychological consequences. These concerns can include:

Feeling of shame and embarrassment: Many women may be afraid of leaking urine in public and therefore avoid social or sports activities.
Impact on relationships: Incontinence can affect emotional and family relationships, and the person may feel unable to participate fully in family activities.
Increased anxiety and depression: problems caused by urinary incontinence can lead to increased feelings of anxiety and depression. These complications can affect the quality of life.
18. Early diagnosis and treatment
Early detection of urinary incontinence can help prevent further problems. Women should pay attention to any signs of incontinence and see a doctor if they notice any symptoms.
Early treatment is usually more successful and can help improve quality of life.
19. The role of nutrition
Proper nutrition can have a great impact on bladder health and urinary control. Some nutritional tips include:
Reduce caffeine intake: Caffeine can irritate the bladder and aggravate incontinence symptoms. Therefore, it is useful to reduce the consumption of coffee, tea and energy drinks.
Adequate hydration: Drinking enough water is essential to maintain overall health and prevent urinary tract infections, but fluid intake should be limited around bedtime.
Paying attention to irritating foods: Some foods such as spicy spices, citrus fruits and sweets can irritate the bladder. Identifying and limiting these foods may help reduce symptoms.
20. Prevention of urinary infections
Urinary tract infections can lead to urinary incontinence. To prevent these infections, you can pay attention to the following points:
Personal hygiene: Regular washing of the genital area and use of appropriate hygiene products can help reduce the risk of infection.
Adequate fluid intake: Drinking enough water helps to empty the bladder and reduce the risk of infection.
Prevention of constipation: Constipation can lead to more pressure on the bladder. Adequate fiber intake and regular exercise can help prevent constipation.
21. Final speech
Urinary incontinence, as a significant problem in women, needs attention and proper management.
Despite the challenges this condition poses, awareness, treatment, and social support can help improve quality of life.
Women should remember that this problem is common and there is no need to feel ashamed or embarrassed.
By visiting a doctor and benefiting from treatment and support solutions, they can gain better control over their condition and continue an active life.
Encouraging conversation about urinary incontinence and providing accurate information can help reduce taboos and increase social acceptance.
Ultimately, with the right support and treatment, many women can improve their quality of life and continue to live happy and healthy lives.
Strengthening the pelvic floor muscles can help improve bladder control and reduce urinary incontinence.
There are several types of exercises that help strengthen these muscles. In the following, we introduce the most important of them:
1. Kegel exercises
These exercises are one of the most effective ways to strengthen the pelvic floor muscles.
How to do:
Identifying the muscles: To identify the pelvic floor muscles, try to stop the flow of urine while urinating. The muscles you use are the pelvic floor muscles.
Stretching: Sit or lie down in a comfortable position. Contract the pelvic floor muscles slowly and hold for 3 to 5 seconds.
Release: Then slowly relax the muscles and rest for 5 seconds.
Repetition: Repeat this exercise 10 to 15 times a day.
2. Bridge
In addition to strengthening the pelvic floor muscles, this exercise also helps to strengthen the abdominal and back muscles.
How to do:
Lie on your back and bend your knees and place your feet on the floor.
Place your hands beside your body.
Slowly lift your hips off the ground so that your body forms a straight line from your knees to your shoulders.
Hold this position for 5 seconds and then slowly return to the starting position.
Repeat this exercise 10 to 15 times.
3. Sitting and getting up (Squats)
This exercise helps to strengthen the pelvic floor muscles as well as leg muscles.
How to do:
Stand with your feet shoulder-width apart.
Slowly go into a sitting position, as if you were going to sit in a chair.
Then slowly return to standing position.
Repeat this exercise 10 to 15 times.
4. Sitting exercises
These exercises can be done at any time and place.
How to do:
Sit in a comfortable chair and put your feet on the floor.
Slowly contract the pelvic floor muscles for 5 seconds and then release.
Repeat this exercise 10 to 15 times.
5. Medicine ball exercises
Using medicine balls to strengthen the pelvic floor muscles can be helpful.
How to do:
Get on your knees and hands and place a small medicine ball between your knees.
Gently squeeze the knees together and then release.
Repeat this exercise 10 to 15 times.
Important points
Breathing: Pay attention to your breathing while doing exercises. Do not hold your breath.
Consistency: For best results, do the exercises regularly.
Consult a doctor: Before starting any new exercise program, it’s best to consult a doctor or physical therapist, especially if you have any specific problems.
conclusion
Pelvic floor muscle strengthening exercises can help improve quality of life and reduce urinary incontinence.
By doing these exercises regularly, many women can increase the strength of their pelvic floor muscles and have more control over their bladder.