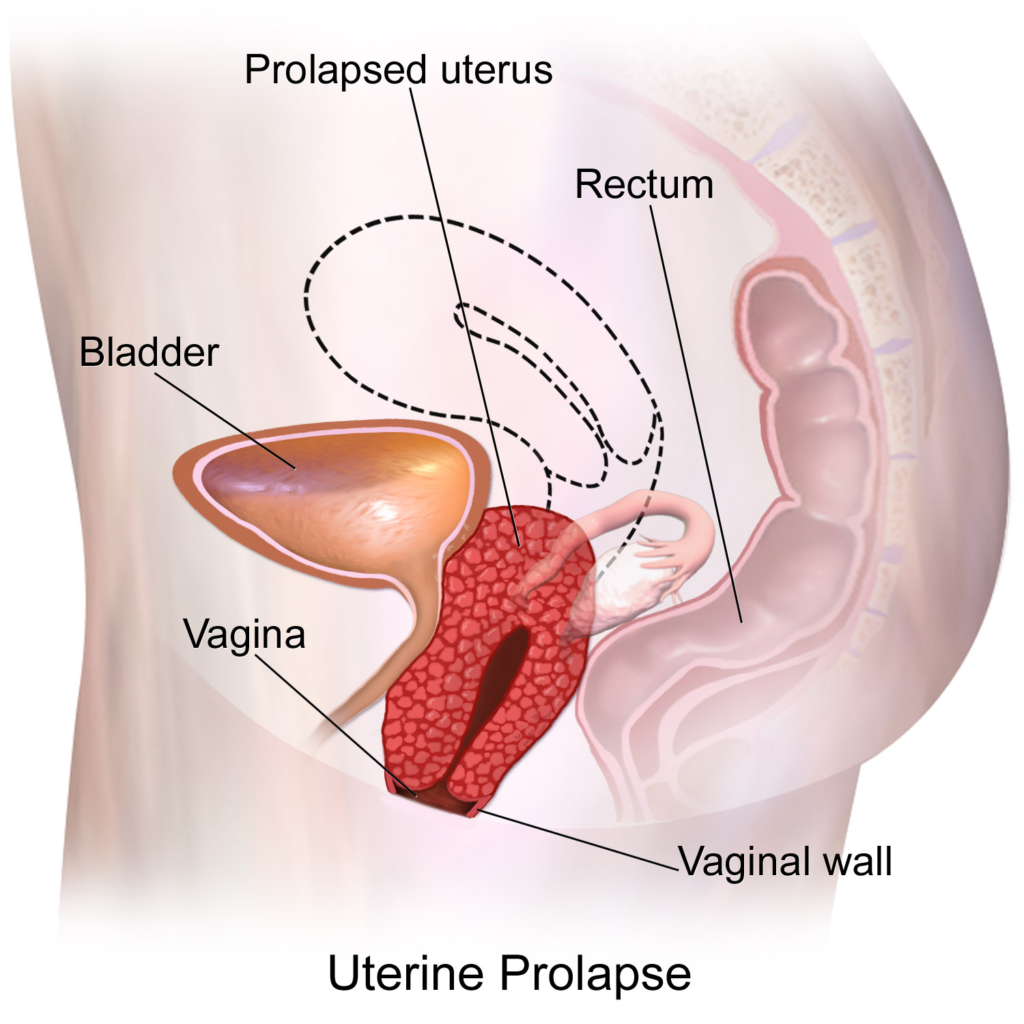
Uterine and bladder prolapse, which is also called pelvic organ prolapse, is a condition in which the uterus or bladder moves down and even out of the body due to weakness or stretching of the muscles and supporting tissues in the pelvic region.
This condition can range from mild to severe, and in more advanced cases, it can cause discomfort and problems with bladder, bowel, and even sexual intercourse.
Causes of uterine and bladder prolapse
The main causes of pelvic organ prolapse include the following:
1. Pregnancy and repeated natural births: Natural births, especially if they are difficult and long, may damage the pelvic muscles and ligaments.
2. Age: With age, the muscles and supporting tissues of the body become weaker and the possibility of sagging increases.
3. Decrease in estrogen levels after menopause: Estrogen helps maintain the health of pelvic tissues, and its decrease can lead to tissue weakness in this area.
4. Constant pressure on the pelvis: such as chronic coughs, constipation and even lifting heavy objects.
5. Obesity: Excess weight can put more pressure on the pelvis.
Symptoms of uterine and bladder prolapse
Prolapse can cause a variety of symptoms, including:
• Feeling of heaviness or pressure in the pelvic area
• Pain in the back and abdomen
• Difficulty emptying the bladder or the feeling of urine remaining after defecation
• Urinary incontinence
• Problems with defecation
• Sensation of a lump or lump in the vagina, especially when standing or exercising
Treatment methods
Depending on the severity of the sagging, different treatments are suggested:
1. Pelvic floor exercises (Kegel): These exercises strengthen the pelvic muscles and can help improve prolapse.
2. Using a pessary: a small device that is inserted into the vagina and helps to hold the organs in place.
3. Hormone therapy: In postmenopausal women, the use of topical estrogen may be helpful.
4. Surgery: In severe cases, surgery can restore the organs to their original place. The type of surgery depends on the condition of the patient and the severity of the prolapse.
Prevention of uterine and bladder prolapse
• Regular exercise and pelvic floor exercises: especially Kegel exercises
• Maintain a healthy weight: Losing weight can reduce pressure on the pelvis.
• Avoiding lifting heavy objects and observing correct lifting techniques
• Prevention of constipation: Consuming enough fiber and water helps to prevent constipation.
Uterine and bladder prolapse is a common problem and can be managed according to doctor’s advice and using appropriate methods.

In the following, it should be mentioned that prolapse of the uterus and bladder occurs in different degrees and its severity can affect the type of treatment and its effect on daily life.
Prolapse is divided into three degrees:
Degrees of uterine and bladder prolapse
1. First-degree prolapse (mild): In this case, the uterus or bladder has moved slightly downward, but is still inside the vagina and usually does not cause many symptoms.
2. Second-degree (moderate) prolapse: In this condition, the uterus or bladder is so low that it may be felt near the opening of the vagina or even outside it.
This stage may cause symptoms such as urinary incontinence, feeling of pressure in the pelvis and discomfort in daily activities.
3. Third-degree (severe) prolapse: In this case, the uterus or bladder has completely protruded out of the vaginal opening.
This type of prolapse usually requires more serious treatments, including surgery.
Impact of falling on quality of life
Pelvic organ prolapse can affect a person’s quality of life. Some of the problems that a person may face are:
• Problems in sexual performance: In some women, a prolapsed uterus or bladder may cause pain or discomfort during sex,
and this can lead to psychological problems and a decrease in self-confidence.
• Urinary and intestinal problems: Due to the displacement of the bladder or other related organs, a person may have urinary incontinence or
even problems in emptying the bladder completely.
• Sleep disorders: the feeling of pressure and discomfort in the pelvis can disrupt night sleep and lead to fatigue and depression.
Combined therapeutic approaches
In cases where the prolapse is moderate to severe, doctors may use a combination of approaches, for example:
• Specialized physiotherapy treatments: physiotherapists specializing in pelvic health can help strengthen pelvic muscles by teaching specialized exercises
and using electrostimulation devices.
• Changes in lifestyle: Patients are advised to take advantage of a healthy lifestyle, including proper diet, proper exercise, and stress management.
• Drug treatments: In some cases, the doctor may use special drugs that help to heal muscles and tissues to reduce symptoms.
Surgical treatment for uterine and bladder prolapse
If non-surgical methods are not effective enough, surgery may be the last option. The type of surgery depends on several factors, including:
• Reconstructive surgery: In this method, the supporting tissues of the pelvic organs are strengthened and the organs are returned to their original place.
• Hysterectomy: In cases where the prolapse is very severe and the uterus is completely protruding, the doctor may recommend a hysterectomy (removal of the uterus).
• Mesh-based surgeries: Medical meshes are sometimes used to strengthen pelvic tissues, but this type of surgery may have complications and should be carefully considered.
Post-treatment care
After treatment (whether surgical or non-surgical), it is very important to follow the post-treatment care to prevent prolapse recurrence. Some of these cares include:
• Perform regular pelvic floor exercises: especially after recovery from surgery
•Avoiding heavy and stressful activities: especially in the first weeks after surgery
Follow-up schedules and periodic check-ups: to ensure that the treatment is working well and there are no signs of the problem returning.
final word
Uterine and bladder prolapse is a common problem, but due to advances in treatment and increased awareness, many people can prevent its complications or manage it well.
Visiting a gynecologist and performing periodic examinations can help to diagnose this problem in time and provide appropriate treatment.

Methods of preventing recurrence of prolapse
After treating prolapse, following some tips can help prevent the problem from returning. These tips include the following:
1. Regular and appropriate exercises to strengthen the pelvic floor: doing Kegel exercises or other pelvic floor exercises continuously can strengthen the pelvic muscles
and prevent sagging again.
2. Maintain proper weight: Excess weight can put more pressure on the pelvic muscles. Losing weight and maintaining proper weight can help reduce pressure on the pelvic organs.
3. Prevention of chronic constipation: Constipation can put a lot of pressure on the pelvis and lead to prolapse again.
Constipation can be prevented by consuming fiber, enough water and regular physical activity.
4. Avoiding lifting heavy objects: Lifting heavy weights or bearing a lot of pressure can weaken the pelvic muscles.
If you need to lift objects, it is better to follow the correct lifting techniques and use the help of others.
5. Going to the doctor for periodic examinations: Even after successful treatment, it is necessary to have periodic examinations with the doctor
to ensure the health of the pelvic muscles and tissues.
Common questions about uterine and bladder prolapse
Here are some frequently asked questions about pelvic organ prolapse and their answers:
• Can uterine or bladder prolapse be treated completely? In many cases, pelvic organ prolapse can be improved with different methods
and even in mild cases it can be completely improved.
But in more severe cases, surgical treatments may be needed and there is a possibility of recurrence.
• Are pelvic floor exercises (Kegel) alone enough for treatment? For mild or early prolapse, pelvic floor exercises can help.
But in more severe cases, additional methods such as pessary or even surgery are needed.
• Does uterine and bladder prolapse only occur in elderly women? No, although pelvic organ prolapse is more common in older women and especially after menopause,
it can happen at any age, especially in women who have had difficult births.
• Do pessaries have special complications? The use of pessaries usually does not have many side effects, but in some people it may cause irritation,
frequent infections or discomfort that requires medical advice.
The importance of counseling and psychological support
Pelvic organ prolapse can have psychological effects on a person. This problem may lead to low self-confidence, problems in marital relationships and even depression.
For this reason, along with physical and medical treatments, it is also important to receive counseling and psychological support.
Talking to a counselor and getting support from family and friends can help a person cope better and recover.
conclusion
Uterine and bladder prolapse is a common problem, especially in older women and women who have had natural deliveries.
Fortunately, this problem can be managed and treated with a variety of methods ranging from pelvic floor exercises to specialized surgeries.
By following preventive measures and performing periodical examinations, the probability of the problem returning can be reduced and a better quality of life can be achieved.
Uterine prolapse is usually diagnosed through a physical examination by a gynecologist.
By examining the symptoms and performing some detailed tests and examinations, the doctor can diagnose the amount of prolapse and suggest suitable treatment methods.
The diagnostic steps include the following:
1. Check medical history and symptoms
The doctor first talks to the patient about signs and symptoms such as pressure or heaviness in the pelvic area, urinary or bowel problems, and any changes in sexual function.
It also examines the history of childbirth, previous surgeries, and related chronic diseases.
2. Physical examination of the pelvis
In the next step, the doctor performs a physical examination of the pelvic area.
This examination usually includes observing and palpating the pelvic organs such as the uterus, bladder, and vagina.
The doctor will ask the patient to strain during the exam (such as moving during a bowel movement) to see if the uterus or other organs come out.
3. Assessment of prolapse severity
Uterine prolapse is divided into different degrees (mild, moderate, severe), and the doctor can determine the severity of prolapse by examining the position of the uterus in the pelvic area.
This evaluation helps the doctor to suggest the best treatment method.
4. Additional tests
In some cases, the doctor may use the following tests for a more detailed evaluation:
Pelvic ultrasound: Ultrasound imaging can help the doctor see more details of the condition of the pelvic organs.
• Cystoscopy: This test is performed to view the inside of the bladder and urethra, especially in cases where a person has urinary problems.
• Urodynamics: If the patient has problems such as urinary incontinence, a urodynamic test may be performed to check the function of the bladder and related muscles.
5. MRI test (in certain cases)
In more complex cases or for a more complete evaluation of the pelvic region, the doctor may use an MRI.
This imaging can provide a more accurate picture of the pelvic organs and supporting tissues and help the doctor formulate a more appropriate treatment plan.
6. Detection of simultaneous prolapses
In some cases, in addition to prolapsed uterus, other pelvic organs such as bladder or rectum may also be prolapsed.
The doctor diagnoses these prolapses and includes them in the treatment plan with careful examination.
Diagnosis result and treatment plan
After completing the diagnosis and assessment of prolapse severity, the doctor determines the appropriate treatment plan.
This program may include pelvic floor exercises, the use of a pessary, hormone therapy, or even surgery, depending on the needs and conditions of the patient.
Final point
Timely diagnosis and seeing a doctor in the early stages of prolapse can help prevent the exacerbation of symptoms and reduce the need for invasive treatments.
Surgery to treat uterine and bladder prolapse can be effective, but like any other surgery, it may have complications and risks. Possible complications of this surgery include the following:
1. General complications of surgery
Infection: There is a risk of infection at the surgical site.
Bleeding: Excessive bleeding may occur during or after surgery.
Damage to surrounding tissues: There is a possibility of damage to nearby organs such as intestines or bladder.
2. Special complications
Urinary leakage: Some patients may experience problems with urinary leakage after surgery.
Sexual problems: Changes in sensation or pain during sex may occur.
Prolapse again: Uterine or bladder prolapse may happen again.
3. Long-term complications
Changes in bladder function: Some patients may have problems urinating or controlling urine after surgery.
Pelvic floor syndrome: In some cases, new pelvic floor problems may develop due to changes in the structure of the pelvis.
4. Psychological complications
Anxiety or depression: Some patients may experience anxiety or depression for various reasons, including physical changes or worry about complications.
conclusion
Before deciding to have surgery, it’s important to fully discuss the benefits and risks with your doctor.
Your doctor can provide detailed information about specific complications and risks associated with your individual condition.
Also, it can be helpful to explore non-surgical options and other treatment methods.
The recovery time after uterine and bladder prolapse surgery can vary depending on the type of surgery, the health status of the person and other factors. In general, recovery may be as follows:
1. Early recovery
• Duration of hospitalization: Most patients can be discharged from the hospital after surgery on the same day or the next day, but hospitalization may be between 1 and 3 days.
• Daily activities: People can usually return to their light daily activities after 1 to 2 weeks.
2. Full recovery
• Vigorous activities: It usually takes 4 to 6 weeks to return to heavy activities and vigorous sports.
• Rest and care: The doctor may recommend that patients avoid vigorous activity, heavy lifting, and sexual intercourse for the first 2 to 6 weeks.
3. Follow-up and examinations
• Post-surgery examinations: The doctor usually examines the patient after 6 to 8 weeks to check the recovery status and possible complications.
Important points
• Follow your doctor’s advice: It is very important to follow your doctor’s instructions regarding post-surgery care.
• Paying attention to warning signs: If you experience any unusual symptoms such as severe pain, excessive bleeding or signs of infection, you should see a doctor.
In general, full recovery may take several months and varies from person to person.